How employers can support employee well-being within an employee benefits program
As defined by the Canadian government: mental health refers to one’s general state of psychological and emotional well-being. We acknowledge this is a complex and nuanced topic, and that an employer’s role in supporting positive well-being extends far beyond the insurance coverage they offer to employees. However, our focus here is on employee benefit products and services that fall under the ‘mental health’ umbrella.
We are often asked “what more can we do” when it comes to mental health coverage. We have outlined the key areas of coverage for mental health and addressed how they should be reviewed, potentially amended or enhanced, and additional layers or adjacent programs you may wish to consider.
Supporting Mental Health: Crisis Response vs Ongoing Care and Support
One thing to consider is an emergency or crisis situation versus an ongoing situation an employee may be struggling with. One may lead to another. While there are many quality resources available for those reaching out during a crisis (there are a plethora of hotlines available to members of various communities, for a wide range of issues or just general support), when an issue requires ongoing professional support, a financial barrier to care may present itself. In this article, we have outlined the various layers of support.
Employee & Family Assistance Program; the First Level of Support
Employee & Family Assistance Programs or EFAPs (also called Employee Assistance Programs or EAPs) are well-known for their ability to provide 24-7 phone-based, online or direct support to members experiencing any sort of life event for which they need assistance. As we’ve written about, they offer benefits to both employers and employees. Most EFAP providers have extensive online resources available on a large variety of topics, and these often do not require membership or a login.
Most plans offer some level of face-to-face or virtual counseling. While this varies depending on the EFAP, they are typically best suited to issues that can be resolved in the shorter-term, or where the member would benefit from referral to relevant online or community resources.
Our experience is that most members who require ongoing support desire to continue with face-to-face or virtual sessions directly with a counsellor of their choosing, who specializes in their area of concern. A downfall of EFAPs can be the inability to continue sessions with the same practitioner, once the limited free sessions expire. In this situation, a member may look to claim under their extended health care program.
Paramedical Practitioners; Reimbursement for Therapist Visits
Paramedical practitioners are a key component of an extended healthcare offering, and depending on the group, may make up a large percentage of overall extended healthcare claims.
While we still see Massage, Physiotherapy and Chiropractor as the top claimed practitioners, those that fall under the ‘mental health’ umbrella have risen in ranking over the past several years. These practitioners include:
- Certified Clinical Counsellor
- Registered Clinical Counsellor
- Registered Professional Counsellor
- Mental Health Therapist
- Psychiatrist
- Psychologist
- Psychoanalyst
- Psychotherapist
- Psychoeducator
- Social Worker
- Marriage and Family Therapist
This list is not inclusive of many other related practitioners that some carriers are willing to include. If you’re unfamiliar with your offering, we recommend reviewing the booklet or contract to determine which practitioners are included; you may want to expand this offering to allow members a greater breadth of choice.
How much paramedical coverage should we provide?
As you may be aware, counselling sessions are extremely expensive, usually well over $100 per visit, depending on the practitioner, type of therapy and region.
A typical plan has $500 of coverage, per practitioner, per person, per year. But keep in mind the providers listed above are usually combined under the dollar limit for “mental health practitioners.”
We often see $750 of coverage these days, and some plans still have lower amounts such as $300. If you do the math, a standard paramedical schedule does not offer many visits to a private therapist.
In an effort to expand the coverage for these categories of practitioners, in recent years we have implemented a higher combined limit (i.e. $1,000 of coverage for these practitioners, while the remainder of practitioners are kept at a lower dollar limit per person per year).
Alternatively, we have provided a specific number of visits, rather than a dollar limit (i.e. 12 visits for mental health practitioners). This is considered a more costly option due to the average per-visit cost.
Health Spending Account dedicated to Mental Health support
For those facing ongoing expenses, for example, routine visits to a therapist, EFAP and paramedical coverage can run out very quickly. To provide an additional layer of support, a Health Spending Account can be used to provide much-needed dollars to employees.
In fact, while barriers to ongoing care due to stigma or lack of resources may have been removed, financial constraints could be the last remaining reason an employee may discontinue therapy, or not seek professional assistance at all.
As you may be aware, Health Spending Accounts can be fully customized these days to include and exclude items, depending on the Employer’s choice. A Health Spending Account can be used to cover mental health-related expenses; however, the employer may choose to define this.
Coinsurance can also be applied (i.e. 60% coverage) with a Health Spending Account, which is an effective tool in directing employees first to their EFAP (potentially), then paramedical coverage under their insured program, and then to their HSA.
Long Term Disability Coverage for mental health claims
Unfortunately, many people find themselves unable to complete the duties of their occupation due to mental health issues. Rest assured, so long as the ‘definition of disability’ within the contract is met, a claim related to mental health can be approved and benefits paid. In fact, a large percentage of claims today are mental health-related, with a larger percentage defined as mental health adjacent.
Members can receive an ongoing monthly income (a disability benefit payment) so long as they continue to meet the definition of disabled. It is important that employers understand this and communicate this to members who may need to explore a long-term disability claim.
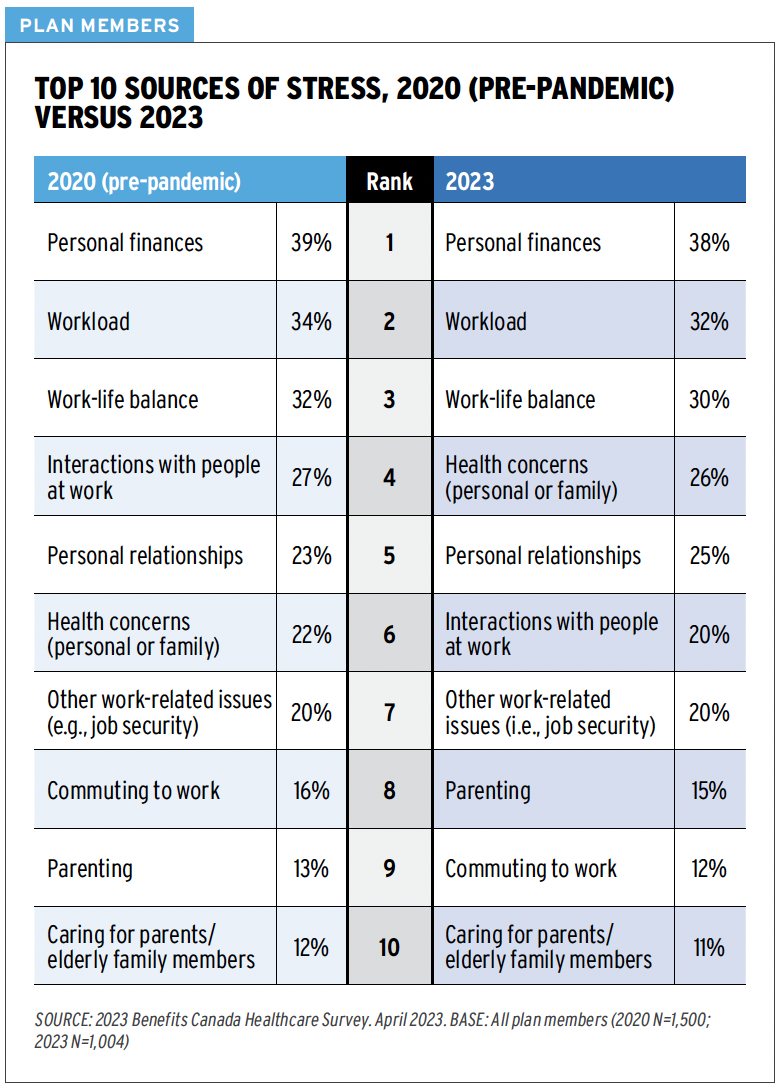
Financial well-being and mental well-being are connected
While we consider this adjacent to the more direct mental health support and benefits detailed above, a groups savings program can play a role in supporting wellbeing. As we have written about, personal finances are their number one source of stress, according to employee surveys.
Implementing an employer-sponsored group savings program provides twofold support: employer funds via an employer contribution to the savings plan, and additionally, education and tools to assist employees in creating a plan and getting control over their finances.
Steps for Employers:
- Ensure an Employee & Family Assistance Program is in place; these are often included within your extended health care plan.
- Review the paramedical offering and ensure appropriate practitioners are included and that coverage levels are as high as affordable to your company.
- Consider a Health Spending Account to provide additional dollars, as well as flexibility and choice
- Ensure employees understand the coverage and how to access support and map out how each layer of coverage works.
- Curate a list (with the help of your advisor!) of good online resources with brief summaries of the support they provide. A simple handout dedicated to this topic, with websites and phone numbers clearly listed, can go a long way.
- Lastly, include details on all of the above as part of onboarding, but also routinely communicate and update your mental health support program.
By offering resources like Employee & Family Assistance Programs, coverage for various mental health practitioners, Health Spending Accounts, and long-term disability coverage, employers can provide additional support for their employees’ mental health and overall well-being.
At the Immix Group, we emphasize the importance of regularly reviewing and communicating the specific benefits offered to employees through their employee benefits program. This ensures they know how to access and utilize these benefits both efficiently and effectively. For any questions about your employee benefits program and whether you can do more to support your employee’s mental well-being, visit us at immixgroup.ca or call us at (604) 688-5559. We love to hear from you!
There are a plethora of free resources and guides available online. Here are a few:
- Government of Canada
- Canada Life: Workplace Strategies for Mental Health
- Manulife: Your Mental Wellness Resource
- Homewood Health: Resources
- Kids Help Phone
- BC’s Hub for Workplace Mental Health
- EAPs- how these programs can benefit both employees and organizations
- 3 Action Steps Employers Can Take to Reduce Employee Financial Stress and Increase Financial Literacy
Top 8 FAQ’s
Mental health refers to one’s general state of psychological and emotional well-being. When employers actively support mental health, they show they care about their employees’ overall well-being, which can lead to a happier, more productive workplace with less absenteeism and stronger company morale.
An EFAP, also known as an Employee Assistance Program (EAP), provides 24/7 phone-based, online, or direct support to employees experiencing life challenges. It offers short-term counseling, referrals to specialized resources, and extensive online materials on various topics, helping employees manage their mental health effectively.
Paramedical practitioners, such as psychologists, psychiatrists, and social workers, provide specialized mental health care. Coverage for these practitioners is a key component of extended healthcare plans. Ensuring a broad range of covered practitioners allows employees to choose the best support for their needs.
Typical plans offer around $500 per practitioner per person per year, but this can vary. Increasing coverage to $750 or more, or offering a specific number of visits (e.g., 12 visits), can provide better support for employees needing ongoing mental health care.
An HSA allows employers to allocate additional funds for employees’ health-related expenses, including mental health services. It can cover costs not fully covered by standard benefits, helping employees to better afford ongoing therapy and other mental health support.
Long-term disability coverage provides financial support to employees unable to work due to mental health issues. If the ‘definition of disability’ in the contract is met and the claim is approved, employees can receive ongoing monthly income, ensuring financial stability during recovery.
Financial stress is a major contributor to poor mental health. Employer-sponsored group savings programs, which include education and tools for financial planning, can alleviate financial stress and support overall well-being.
Employers should ensure EFAPs are in place, review and enhance paramedical coverage, consider implementing HSAs, communicate coverage details clearly, provide accessible resources, and regularly update and promote the mental health support available.
Read more:

Lindsay Byrka BA, BEd, CFP
Vice President, Immix Group: An Employee Benefits Company
A Suite 450 – 888 Dunsmuir St. Vancouver V6C 3K4
O 604-688-5262 E lindsay@immixgroup.ca
W www.immixgroup.ca